Gladstone-UCSF Institute of Genomic Immunology Symposium
|
|   | |||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||
FREEDOM with honesty, justice and courage.. COMPASSION with dignity, humour, and tolerance.. KNOWLEDGE with effort, perseverance and sharing.. LOVE with peace and harmony towards all life on Earth. A science-based international free press humanitarian organization.. created in 1972.. human4us2.blogspot.com...
|
|   | |||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||
GENTLE PEOPLE:
It has been over a year now since the covid-19 virus created an international pandemic of sickness and death. As of this date, Sunday, October 10, we continue to live in fear of the deadly virus but thanks to new and quickly developed and distributed vaccines, millions of us have survived the pandemic.
THE BIG QUESTION NOW IS, ARE WE FINALLY SAFE?
SADLY, THE ANSWER IS NO! THE VIRUS HAS MUTATED AND WE NEED TO CONTINUE DEVELOPING NEW AND BETTER METHODS TO BLOCK COVID AND OTHER DANGEROUS VIRUS FROM PROLIFERATING...
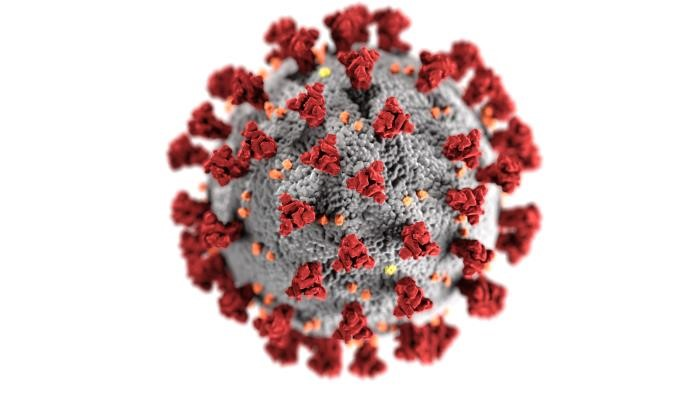
COVID-19 is caused by the coronavirus SARS CoV-2, previously called 2019-nCoV. It belongs to the Coronaviridae family and is broadly distributed in humans and other mammals. hCoV-229E, OC43, NL63 and HKU1 are some of the known coronaviruses that cause mild respiratory diseases unlike SAR-CoV and MERS that cause severe to fatal respiratory diseases [1].
Why is SARS-CoV-2 spreading faster than its two ancestors? Why is SARS-CoV-2 lethal? Recent publications have shown that there are differences in their genome structure and immunological response to SARS-CoV-2 infection. The key markers involved in these interactions include Spike protein (S), Nucleocapsid (N), ACE-2 receptor, FURIN protease in addition to the cytokines.
Spike Protein (S): SARS-CoV2 enters the cells through the Spike mediated interaction with the ECD domain of the ACE2 cell receptor. (A recombinant fusion protein (RBD of Spike protein and ECD of membrane protein) can be a great tool to investigate this interaction.
Learn more about the purified recombinant Spike Protein (S).
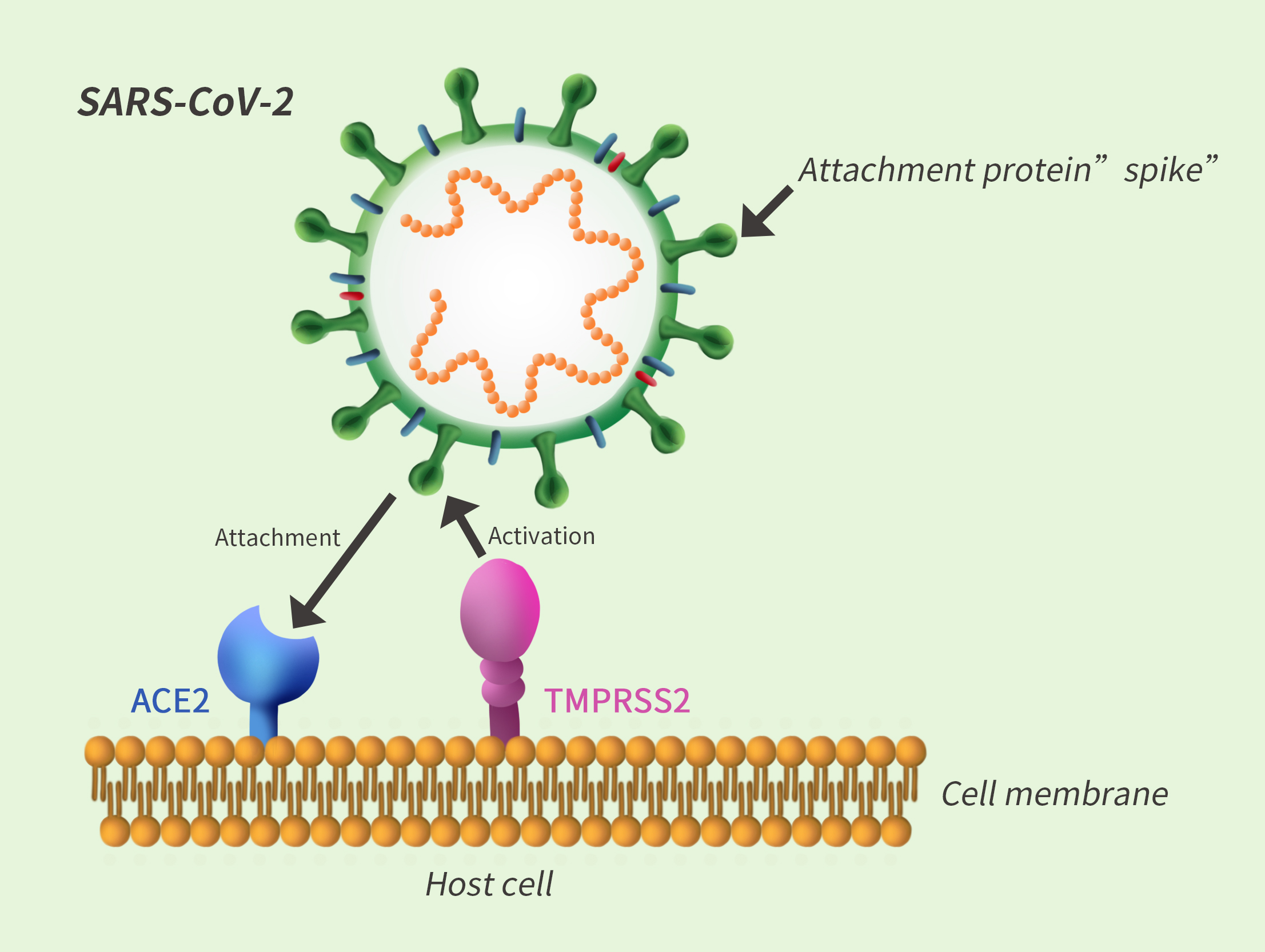
Transmembrane Serine Protease 2 (TMPRSS2): This is a serine protease that cleaves and activates the viral spike glycoproteins which facilitates virus-cell membrane fusions. A recent study showed that SARS-CoV-2 needs both ACE2 receptor and serine protease TMPRSS2 for protein priming to enter the cell.[2]
Tools for analyzing TMPRSS2
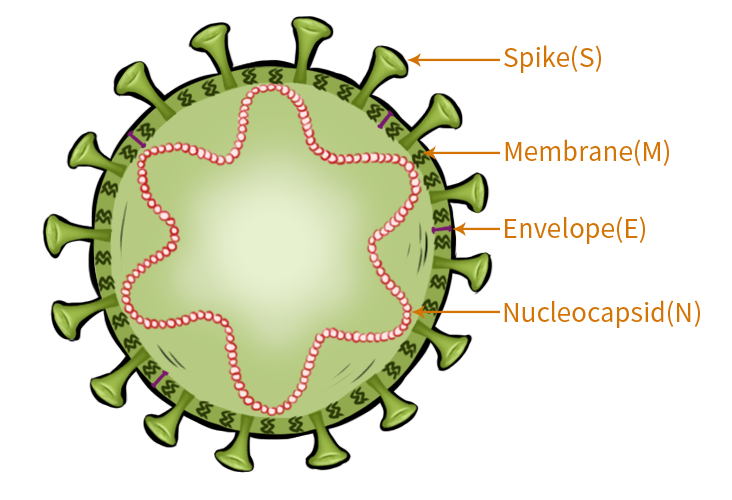
Nucleocapsid: The nucleocapsid phosphoprotein packages the viral genome into a helical ribonucelocapsid, thus playing a crucial role in viral self-assembly.
Tools for analyzing the Nucleocapsid
ACE-2 receptor: ACE-2 is the host cell receptor responsible for mediating infection by SARS-CoV-2.
Tools for analyzing ACE-2 protein
Find out more about the additional ACE-2 specific tools here

Furin: It is a protease present in many human organs that recognizes and activates a specific site on the SARS-CoV-2 Spike protein, thus facilitating a tighter binding to the ACE-2 receptor and might play a role in the higher infection rate [3].
How can you analyze Furin? Learn about the tools for analyzing Furin.
ATTENTION WORLD GOVERNMENT LEADERS!
YOUR SCHOOLS ARE CURRENTLY TRAINING CHILDREN TO WORK FOR BIG BUSINESS. THIS MUST STOP! CHILDREN NEED TO CHANGE AND GREEN THE ECONOMY TO HELP PRESERVE NATURE. WE NEED AN ECONOMY BASED ON NATURE AND NOT AN ECONOMY BASED ON OIL AND GAS AND POLLUTING INDUSTRY.
EVERY SCHOOL MUST HAVE : TREES, VEGETABLES, AND FLOWER GARDENS, WITH CHILDREN LEARNING ABOUT AND CARING FOR PLANTS. WHY? BECAUSE WITHOUT NATURE LIFE CEASES TO EXIST AND TODAY NATURE IS BARELY SUSTAINING THE LIFE OUR POLLUTING INDUSTRIAL ECONOMY IS DESTROYING! THIS IS NOT AN OPINION OR A THEORY, IT IS A FACT.
WE NEED PEOPLE WHO HAVE LEARNED IN CHILDHOOD AS MUCH BOTANY AND BIOLOGY AND WAYS TO PROTECT THE ENVIRONMENT AS IS HUMANLY POSSIBLE AND WHO ARE NOT AFRAID TO TAKE ACTION. IT BEGINS BY CHANGING THE SCHOOL ENVIRONMENT AND IT ENDS WITH THE CREATION OF A BEAUTIFUL NATURAL ENVIRONMENT WE CAN ALL BE PROUD OF.
N.J.R.
THE FOLLOWING ARE MORALLY WRONG AND ETHICALLY EVIL...
1. THE MURDER OF AIR BREATHING FRIENDLY DOLPHINS AND WHALES FOR THEIR MEAT AND OIL.
2. THE POLLUTION OF AIR AND WATER WITH OIL AND PLASTIC AND GAS.
3. GENETICALLY CONVERTED SEEDS THAT RESIST POLLUTION AND PESTICIDES AND ALLOW FARMERS THE USE OF DANGEROUS PESTICIDES WHICH CONSEQUENTLY KILL SONG BIRDS AND BEES.
Existing measures for infectious disease control face three ‘universal’ barriers:
(i) Deployment (e.g. reaching the highest-risk, infectious ‘superspreaders’ who drive disease circulation)
(ii) Pathogen persistence & behavioral barriers (e.g. adherence)
(iii) Evolution (e.g. resistance and escape)

These barriers exist because pathogens are dynamic—they mutate and transmit—while existing therapies are static, neither mutating nor transmitting. To surmount these barriers, we have proposed a radical shift in therapeutic paradigm toward developing adaptive, dynamic therapies (Metzger et al. 2011). Building off data-driven epidemiological models, we show that engineered molecular parasites, designed to piggyback on HIV-1, could circumvent each barrier and dramatically lower HIV/AIDS in sub-Saharan Africa as compared to established interventions.
Above: A representative model for how a small 'core groups' of high-risk 'superspreaders' (e.g. commercial sex workers and their clients) drove the HIV-1
epidemic in sub-Saharan Africa along the trans-Africa highway in the 1980s. These hard-to-reach groups--often stigmatized and disenfranchised--disproportionately drive disease spread and can be described by the Pareto '80/20' rule - where 80% of new infections are driven by 20% of the population.
Above: Theoretical model of how Therapeutic Interfering Particles (TIPs) would act to reduce the burden of HIV on a population-wide scale. Small blue "pools" of infection represent a local reduction in HIV by the TIP, and are rapidly spread by a "superspreader population".
These molecular parasites essentially steal replication and packaging resources from HIV within infected cells thereby generating Therapeutic Interfering Particles (TIPs)[1] which deprive HIV of critical replication machinery thereby reducing viremia. The fundamental departure from conventional therapies is that TIPs are under strong evolutionary selection to maintain parasitism with HIV and will thus co-evolve with HIV, establishing a co-evolutionary ‘arms race’ (Rouzine and Weinberger, 2013).
Like Oral Polio Vaccine, (OPV)—currently used for the W.H.O. worldwide polio-eradication effort—TIPs could also transmit between individuals, a recognized benefit for OPV. TIP transmission would occur along HIV-transmission routes (via identical risk factors), thereby overcoming behavioral issues and automatically reaching high-risk populations to limit HIV transmission even in resource-poor settings.
For review: Notton et al. Current Opinion in Biotechnology 2014.
Papers of note: Metzger, Lloyd-Smith, and Weinberger. PLoS Computational Biology 2011 (videos above) and Rouzine and Weinberger. Journal of Virology 2013 (Linked above).
[1] TIPs are a distinct form of defective interfering particles (DIPs) engineered to have a basic reproductive ratio (R0) > 1.
| ||||||||||||||
Some Vaccines Last a Lifetime. Here’s Why Covid-19 Shots Don’t.
Researchers have calculated a key number—the threshold of protection—for other vaccines. Covid-19’s is still a mystery.
Why don’t Covid-19 vaccinations last longer?
Measles shots are good for life, chickenpox immunizations protect for 10 to 20 years, and tetanus jabs last a decade or more. But U.S. officials are weighing whether to authorize Covid-19 boosters for vaccinated adults as soon as six months after the initial inoculation.
The goal of a vaccine is to provide the protection afforded by natural infection, but without the risk of serious illness or death.
“A really good vaccine makes it so someone does not get infected even if they are exposed to the virus,” said Rustom Antia, a biology professor at Emory University who studies immune responses. “But not all vaccines are ideal.”
The three tiers of defense, he said, include full protection against infection and transmission; protection against serious illness and transmission; or protection against serious illness only.
The effectiveness depends on the magnitude of the immune response a vaccine induces, how fast the resulting antibodies decay, whether the virus or bacteria tend to mutate, and the location of the infection.
The threshold of protection is the level of immunity that’s sufficient to keep from getting sick. For every bug, it’s different, and even how it’s determined varies.
“Basically, it’s levels of antibodies or neutralizing antibodies per milliliter of blood,” said Mark Slifka, a professor at Oregon Health & Science University.
(T-cells also contribute to protection, but antibodies are easier to measure.)
A threshold 0.01 international units per milliliter was confirmed for tetanus in 1942 when a pair of German researchers intentionally exposed themselves to the toxin to test the findings of previous animal studies.
“One of them gave himself two lethal doses of tetanus in his thigh, and monitored how well it went,” Dr. Slifka said. “His co-author did three lethal doses.”
Neither got sick.
A threshold for measles was pinned down in 1985 after a college dorm was exposed to the disease shortly after a blood drive. Researchers checked antibody concentrations in the students’ blood donations and identified 0.02 international units per milliliter as the level needed to prevent infection.
With these diseases, the magnitudes of response to the vaccines combined with the antibodies’ rates of decay produce durable immune responses: Measles antibodies decay slowly. Tetanus antibodies decay more quickly, but the vaccine causes the body to produce far more than it needs, offsetting the decline.
“We’re fortunate with tetanus, diphtheria, measles and vaccinia,” Dr. Slifka said. “We have identified what the threshold of protection is. You track antibody decline over time, and if you know the threshold of protection, you can calculate durability of protection. With Covid, we don’t know.”
Historically, the most effective vaccines have used replicating viruses, which essentially elicit lifelong immunity.
Measles and chickenpox vaccines use replicating viruses.
Non-replicating vaccines and protein-based vaccines (such as the one for tetanus) don’t last as long, but their effectiveness can be enhanced with the addition of an adjuvant—a substance that enhances the magnitude of the response.
Tetanus and hepatitis A vaccines use an adjuvant.
NEWSLETTER SIGN-UP
Coronavirus Briefing and Health Weekly
Get a morning briefing about the coronavirus pandemic three times a week and a weekly Health newsletter when the crisis abates.
T he Johnson & Johnson and AstraZeneca Covid-19 vaccines use non-replicating adenovirus and don’t contain an adjuvant. The Pfizer and Moderna messenger RNA Covid-19 vaccines, which work differently, don’t contain any virus at all.
Complicating things further, viruses and bacteria that mutate to escape the body’s immune response are harder to control.
Measles, mumps, rubella and chickenpox hardly mutate at all, but at least eight variants of SARS-CoV-2, the virus that causes Covid-19, have been found, according to the British Medical Journal.
“It does make it more complicated for the vaccine to work,” Dr. Slifka said. “You’re chasing multiple targets over time. Flu also mutates. With flu, we’ve adjusted by making a new flu vaccine each year that as closely as possible matches the new strain of flu.”
SHARE YOUR THOUGHTS
When do you expect to get your Covid-19 booster shot? Join the conversation below.
To comment, you’ll need to be on WSJ.com
F lu vaccines can offer protection for at least six months.
Setting aside the complexities of crafting an effective vaccine to combat a shape-shifting virus, some hope has revolved around the possibility of defeating Covid-19 by achieving herd immunity, but, according to Dr. Antia, the way coronaviruses infect the body makes that challenging.
“Vaccines are very unlikely to lead to long-lasting herd immunity for many respiratory infections,” Dr. Antia said. “The herd immunity only lasts for a modest period of time. It depends on how fast the virus changes. It depends on how fast the immunity wanes.”
Part of the problem is that coronaviruses replicate in both the upper and lower respiratory tracts.
“We have good circulation in our lungs and body, but not on the surfaces of our nostrils,” Dr. Slifka said. “We can block severe disease because there are antibodies in the lower respiratory tract.”
But the risk of low-level infections in the upper respiratory tract can persist.
Moving forward, Covid-19 vaccines will be updated to combat variants of the virus, and according to researchers at Imperial College London, the next generation of vaccines might also focus on enhancing immunity in the moist surfaces of the nose and lungs.
In the meantime, avoiding the slippery virus might require another shot.
Covid-19 Vaccines
Related coverage, selected by the editors
What to Know About Biden's Vaccine Mandate
CHAT GPT LINKS CANCER TO MICROPLASTIC CONTAMINATION. " MICROPLASTICS ARE COMPOSED PRIMARILY OF SYNTHETIC POLYMER MATERIALS - THAT IS,...