DEAR DR. LEOR WEINBERGER:
Leor Weinberger, PhD, senior investigator and virologist has pioneered an innovative approach to fighting the spread of viral pathogens. His approach is called therapeutic interfering particles or (TIPs), which could be an alternative to a vaccine. He also directs the Center for Cell Circuitry.
"Prevention
A Gladstone team is investigating the potential of an innovative alternative to a vaccine. Therapeutic interfering particles (TIPs) could turn the tables on the virus by hijacking its machinery to transform virus-infected cells into factories that produce more therapeutic particles than virus, slowing its spread.
Dr. Leor Weinberger has developed a new approach to fight the spread of viruses. It is called therapeutic interfering particles (TIPs) and could be an alternative to a vaccine. TIPs are defective virus fragments that mimic the virus but are not able to replicate. They combat the virus by hijacking the cell machinery to transform virus-infected cells into factories that produce TIPS, amplifying the effect of TIPs in stopping the spread of virus. TIPs targeting COVID-19 would transmit along the same paths as the virus itself, and thus provide protection to even the most vulnerable populations.
Treatment
Gladstone researchers mapped interactions between human host cell proteins and the virus, and are now using this information to identify therapeutic targets. Others are screening libraries of FDA-approved drugs and testing their effects on the virus in human lung “organoids” and human heart cells. Additional projects include investigating how the virus affects the brain, leading to cerebrovascular complications and stroke, and studying ways to rejuvenate the immune system to improve its ability to fight infection.
Diagnostics
Gladstone scientists are collaborating to develop a CRISPR-based method to rapidly measure COVID-19 RNA. By combining the technique with smartphone technology, they aim to develop a diagnostic that could deliver rapid results and be widely deployed even far from traditional labs, such as in airports and other ports of entry, and in remote communities throughout the world. Another team is applying machine learning to discover biomarkers that will predict which patients are most likely to experience severe disease, and which may have an asymptomatic course."
------------------------------------------------------
How does coronavirus infect humans?
In mammals, such as humans, DNA contains genetic instructions that are transcribed—or copied—into RNA. While DNA remains in the cell’s nucleus, RNA carries the copies of genetic information to the rest of the cell by way of various combinations of amino acids, which it delivers to ribosomes. The ribosomes link the amino acids together to form proteins that then carry out functions within the human body.
Many diseases occur when these gene expressions go awry.
What does RNA stand for?
RNA stands for ribonucleic acid.
What is RNA?
RNA delivers the genetic instructions contained in DNA to the rest of the cell.
COVID-19, short for “coronavirus disease 2019,” is caused by the novel coronavirus SARS-CoV-2. Like many other viruses, SARS-CoV-2 is an RNA virus. This means that, unlike in humans and other mammals, the genetic material for SARS-CoV-2 is encoded in ribonucleic acid. The viral RNA is sneaky: its features cause the protein synthesis machinery of our cells to mistake it for RNA produced by our own DNA.
While SARS-CoV-2 is a new coronavirus, “it likely replicates and functions similar to related coronaviruses that infect animals and humans,” says Douglas Anderson, an assistant professor of medicine in the Aab Cardiovascular Research Institute and a member of the Center for RNA Biology, who studies how RNA mutations can give rise to human disease.
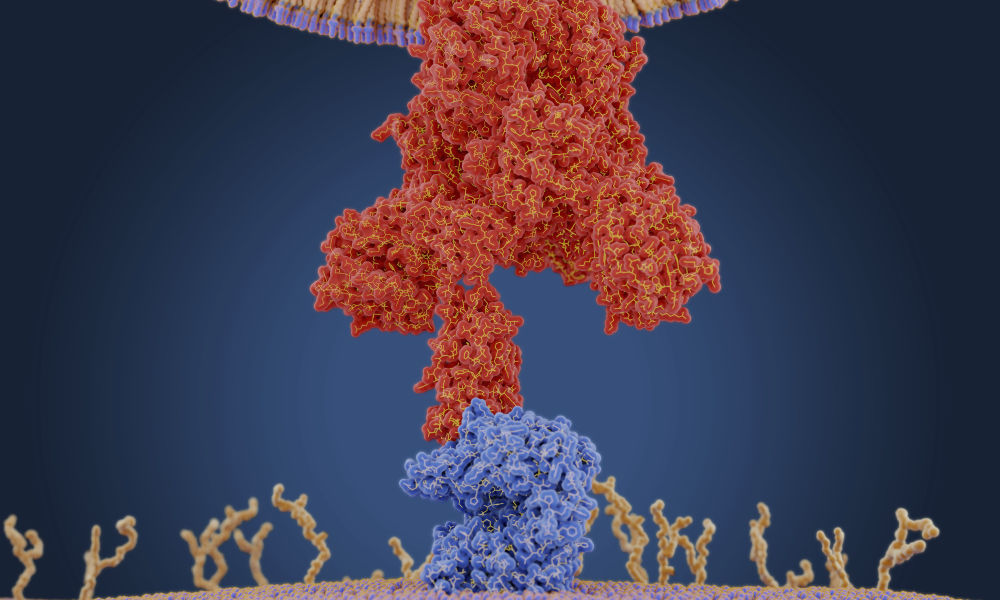
A graphic created by the New York Times illustrates how the coronavirus that causes COVID-19 enters the body through the nose, mouth, or eyes and attaches to our cells. Once the virus is inside our cells, it releases its ribonucleic acid. Our hijacked cells serve as virus factories, reading the virus’s ribonucleic acid and making long viral proteins to compromise the immune system. The virus assembles new copies of itself and spreads to more parts of the body and—by way of saliva, sweat, and other bodily fluids—to other humans.
“Once the virus is in our cells, the entire process of infection and re-infection depends on the viral RNA,” Maquat says.
“Understanding RNA structure and function helps us understand how to throw a therapeutic wrench into what the COVID-19 RNA does—make new virus that can infect more of our cells and also the cells of other human beings,” says Lynne Maquat, professor of biochemistry and biophysics at the University of Rochester Medical Center and the director of Rochester’s Center for RNA Biology.






